BACKGROUND
Chronic venous insufficiency (CVI) is common in the United States and occurs in up to 40% of the population.1–3 CVI affects the venous system and manifests as lower-extremity edema, pain, and, in severe cases, ulcers.4 Untreated or poor management of CVI leads to a decrease in the patient’s quality of life and interferes with activities of daily living.5 The healthcare costs of a conservative treatment regimen, including ulcers and edema, on average exceed $2400 per month, or more than $5500 per episode.6–8 Collectively, US healthcare costs for CVI exceed $4.9 billion annually.9
The use of compression therapy is part of the standard treatment protocol for CVI.10–12 A novel 2-layer bandage system (2LB) has been shown to be safe, efficacious, and well-tolerated by patients for the treatment of CVI.13–18 However, there is limited economic evidence regarding the use of a 2LB system. The objective of the study was to estimate the total cost per response (CPR) for edema resolution and wound healing of patients with CVI treated with a 2LB system as part of their overall treatment regimen.
METHODS
Clinical Data
The clinical data were obtained from a recently published, prospective, multicenter study.19 This study recruited all CVI patients presenting with a venous leg ulcer or edema in which the physician made the clinical judgment to treat with a compression system. A 2LB system was used per the manufacturer’s instructions for use, and all treatment decisions were made by the patient’s physician. Patients were followed in an outpatient setting for a maximum of 6 weeks (average, 27 days). All patients were treated with a 2LB system for the duration of the study. The 2LB system components were a padded inelastic bandage with short elongation and an elastic bandage with lengthy elongation. The system provides a visual indicator to facilitate the proper application and achieve the desired pressure. The system can be worn 24 hours a day for up to 7 days per the instructions for use.13
The study comprised a total of 702 patients (56% female) and included 491 cases of edema and 414 wounds. Bandages were typically changed 1 or 2 times a week (51.7%). For those with wounds, the median duration of the wounds was 42 days, and the median size at the initial visit was 3.5 cm2. Wound healing occurred in 128 of the 414 wounds (30.9%) within the 6-week study period. The proportion of patients with edema that resolved at the end of the study period was 67.1%. All data were publicly available, and the study was deemed exempt from institutional review board review.
Cost and Utilization Data
The cost and utilization data were obtained from a pragmatic literature review. A search of English-language articles from January 2019 to January 2023 was performed in PubMed and Google Scholar for the model parameters. The articles were reviewed based on applicability, recency, and quality by a single reviewer. In the event of more than one study meeting the criteria, a pooled analysis was applied to identify the midpoint value used for the analysis. The cost and utilization data consisted of US national average patient-level data to allow for the results to be applied to a typical health system.
Modeling Strategy
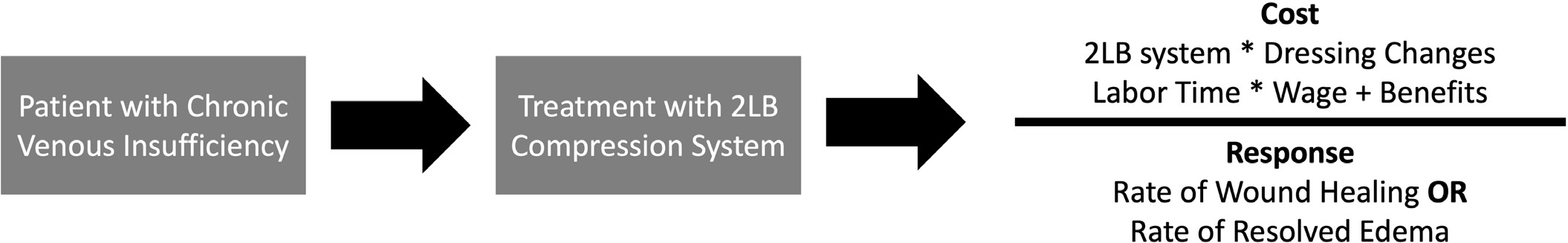
A patient-level probabilistic decision tree model was developed to estimate the incremental CPR for the 2LB system (Figure 1). The perspective of the model was an outpatient treatment center in the United States. The cost parameters included the cost of the 2LB system and the medical technician’s time to apply the 2LB. The outcome measures were the percentage of edema resolved and the percentage of wounds healed at the conclusion of the follow-up period. The CPR was calculated with the following formula for edema resolved and wound healed:
CPR=∑C2LB/Outcome2LB
where C2LB is the summation of the costs of the 2LB system, and Outcome2LB is either the percentage of edema resolved or wound healed. Each model was performed separately, with the only difference being the outcome variable. A total of 10 000 patients were simulated. The base case model values were varied based on the reported ranges shown in Table 1. The models were developed using Treeage Software (Williamstown, Massachusetts). All data used in the model were publicly available in the literature.
RESULTS
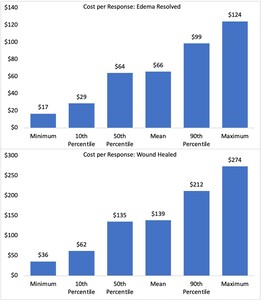
Figure 2 (top panel) and Table 2 show the probabilistic model results to resolve edema using the 2LB system. The mean expected incremental CPR was $65.67. Based on 10 000 simulated patients, the cost to resolve edema ranged from $16.67 to $124.32. The associated cost of the 2LB system over the study period ranged from $10.00 to $92.00, and the probability of resolving the edema ranged from 60% to 74%.
Figure 2 (lower panel) and Table 3 show the probabilistic model results in healing one wound. After 10 000 simulated patient trials, the mean expected incremental CPR was $138.71 and ranged from $35.71 to $273.53. The associated cost of the 2LB system over the study period ranged from $10.00 to $92.00, and the probability of healing the wound ranged from 28% to 34%.
DISCUSSION
This study found the CPR for edema resolved or wound healed was expected to be approximately $66 or $139, respectively. The CPR approach is an effective means to evaluate an intervention because it combines the additional costs of the intervention, 2LB, with the benefit provided by the intervention. The result is more indicative of the overall costs after adjusting for patients who do not benefit from the intervention.
The overall costs to treat CVI run in excess of $5500.6–8 Thus, after adjusting for treatment failures, the use of a 2LB system was expected to account for 1% of the total cost to resolve edema or 3% of healing a wound. This cost is negligible in the overall treatment costs of patients with CVI.
The insignificant cost of the 2LB system should emphasize the safety, efficacy, and patient satisfaction of the 2LB system. A randomized controlled trial of a 2LB system and 4-layer bandage (4LB) system found that 2LB was safe and as effective as the 4LB and easier to apply.13–15 Appropriate pressure has been shown to be maintained with the 2LB system.16,22–24 Patient satisfaction with the 2LB system was 70% compared with 12% with the 4LB system, which led to increased compliance with the 2LB system.22 Finally, the average pain reduction fell by 67% using a visual analog score.19
Limitations
The results of this study were based on clinical data from a noncomparative observational study. Therefore, comparisons to other bandage systems were not possible. However, this study was a large prospective, multicenter study, which provided a real-world setting to conduct an economic evaluation. Second, this study examined the incremental costs of adding a 2LB system into the standard CVI treatment protocol. It was not intended to provide a total cost to treat a patient with CVI. Finally, this study was conducted from an outpatient clinic perspective and may not be generalizable to other sites of care.
CONCLUSION
This study provides economic evidence for using a 2LB system for the treatment of CVI in the outpatient setting. This study complements previous studies demonstrating the efficacy, safety, and increased patient satisfaction of a 2LB system. The use of a 2LB system should be considered an added economic value to the management of CVI.
Disclosures
The author has a consulting relationship with Urgo Medical North America (UMNA).
Funding
Financial support for this research was provided in part by Urgo Medical North America (UMNA). UNMA had no input on the study design, analysis, results, or manuscript.
Ethics Approval and Data Availability
This research used publicly available secondary data.